The Influenza pandemic in 1918 could be considered to be the fatal event in human chronicle constituting about (50 million or More deaths, which could be equated to in magnitude of 200 million in global population today). For more than a century, it has stood as a benchmark against which all other pandemics and disease emergences have been measured. As scientist across the globe remembers the 1918 pandemic, there is another global pandemic and infectious-disease – novel coronavirus infectious disease (Covid-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) found in December 2019 in Wuhan, Hubei Province, China, for which the infection present pneumonia-like symptoms. This could be considered as the first modern pandemic even though speculations thought Ebola outbreak in West Africa could qualify as such.
The Coronavirus outbreak has summon all of humanity against the virus. It negative effect on humanity that is health, wealth, businesses and well-being has already been enormous. This is synonymous to a world war except in this cases all of humanity appears to be on one side to fight it. The novel Coronavirus was identified on January 7th, 2020 by the Chinese Centre for Disease Control as it was rapidly spreading. Such virus was identified as SARS-Cov-2, named for its resemblance to SARS-Cov, a virus identified in 2003. The disease was initially named 2019-nCoV Pneumonia and later Covid-19 by World Health Organization (WHO) on 11th February, 2020. Covid-19 was traced to the local Huanan seafood, wholesale market where most of the victims of Covid-19 lived or worked.
In the early stages of Covid-19 infection, most patients presented with symptoms of fever, dry cough and shortness of breath that may rapidly result in severe respiratory distress syndrome, respiratory failure, multi-organ failure and death. Among cases reported in Iran and U.K, the www.dailymail.co.uk has reported that patients have newer symptoms such as fatigue, insomnia and lose of smell with entirely absence of fever though 70% of cases could present symptoms described by the WHO.
By the end of January, the virus had been exported to several countries in Europe and rapidly spreading resulting in the World Health Organization (WHO) to declare the outbreak as a Public Health Emergency of International Concern on 30 January 2020, guided by the International Health Regulations (2005)
The Statistics
As of May 11, 2020, the rapidly spreading virus had been reported in 213 countries, areas or territories as claimed by WHO with a cumulative reported confirmed cases 4, 102,955 resulting in 781,109 recoveries with Centre for systems Science and Engineering at John Hopkins University reporting a global death of 282, 719. The highest of the confirmed cases is seen in the Americas and European region with Africa reporting the least of the infection rate, consisting about 53 countries reporting 1.55% of the global confirmed cases thus 60, 657 confirmed cases, 2, 223 deaths and 20, 792 recoveries noted by the Africa Centre for Disease Control (Africa CDC) as of May 10, 2020. And the spread of the virus is still accelerating in many African countries on average at 30% every week. The WHO has purged the global risk assessment level as Very high risk.
AFRICA, WEST AFRICAN AND GHANA IN PERSPECTIVE
The African region experiences around 100 public health events annually, of which 80% are caused by infectious diseases noted by WHO. Although only a portion of these public health events are caused by emerging and dangerous pathogens (EDP), recurring outbreaks of diseases such as Ebola Virus Disease (EVD) and Dengue Fever/Dengue Haemorrhagic Fever etc. are a feature of the regional situation and in recent times the global outbreak of SARS-CoV-2 could not be rule out. The health impact of COVID-19 probably differ in African settings as compared to countries in Europe or Asia. This is due to demographic, epidemiological, environmental, socio-economic and behavioural phenomenons. West Africa countries especially Guinea, DR Congo, Sierra Leon and Liberia having dealt with 2014/2015 deadly Ebola pandemic in the region have been faced with the challenges of SARS-CoV-2. Perhaps, they could better deal with it as the regional organization ECOWAS was at the forefront of the Ebola outbreak due to the fact that WHO in then times delayed response decisions. Although using the global parameters as benchmark, cases in Africa in general is very low, however, researches have proven that the continent continue to record cases on daily basis causing rise in daily cases especially in West African countries although claims has it that corona virus perhaps not likely to be able to survive in West Africa due to the tropical climate in the regions. Notwithstanding, such calms cannot be ascertained although fatality rate is at it low side compare to temperate regions like Europe.
An assessment of global health security capacities in 2019 published by the Johns Hopkins Center for Health Security demonstrated that sub-Saharan Africa faces significant challenges in its ability to respond to health emergencies. The assessment went further noting almost the entire African continent as “least prepared” to treat the sick and protect health care workers, and claim most countries lack the equipment and practices in infection control. A report published in the Lancet pointed out in agreement with the Johns Hopkins Centre for Health Security, stating that nearly three-fourths of African countries have influenza pandemic preparedness, on the contrary, majority are outdated and considered inadequate to deal with a global pandemic.
Nonetheless, African Union member states under the guidance of the Africa Centres for Disease Control and Prevention have strengthen testing capacities in over 30 African countries including genome sequencing to understand the virus specific strain in each country.
Dealing with Ebola epidemic in the past, West Africa could tell how pandemic in the modern era looks like and this could positioned the West Africa countries to better deal with the current outbreak of SARS-CoV-2 amidst scarce resources yet have step up preparedness protocols against the disease. This could be confirmed by the director of the Nigeria Center for Disease Control, Chikwe Ihekweazu, noting that Ebola outbreak has taught [us] the ECOWAS region, a lot of lessons. In Africa the concept of solitude hence social distancing is not of common norms. About 56 per cent of Africa’s urban population live in slums where it is not possible to follow WHO recommendations on regular hand washing, social distancing and avoiding crowded places. Residents often live hand to mouth through informal jobs that require contact with others, and staying at home is not an option. Lockdowns in such contexts are not feasible.
Emerging data based on a study of close to 2,000 residents living under lockdown in five slums in Kenya indicate that: Over 75 per cent of residents left their homes an average of three times in 24 hours; Though 95 per cent of public areas have hand-washing stations, 32 per cent of households cannot afford extra soap for hand washing and 84 per cent cannot afford sanitizer; Face masks were used often, at levels reportedly as high as 73 per cent, however, 19 per cent were unable to afford them; The biggest currently unmet need, reported by 76 per cent, was food, with 98 per cent reporting that the situation was a result of the impact of COVID-19, this could be similar situation or a little better in across other Africa countries.
Most countries in West Africa have deployed a non-pharmacological approach in curbing the disease. This has resulted in banning social activities ranging from community gatherings, funerals and religious activities. Schools have been closed, most markets have also been closed except few ones are open to maintain probably the food supply chain.
As of May 3, 2020, the Africa CDC has reported that, on physical distancing measures, 43 Africa countries have implemented full border closure and among these some allows cargo, freight and emergency entry/exit while others allows residents/citizens, but borders are imperatively closed, 7 countries have issue international air traffic closures, 2 implemented travel restrictions to and from specific countries and 3 install entry/exit restrictions. In the light of this, all 54 member states of the African Union instituted mandatory quarantine for all travellers and or travellers from high risk countries and have instituted a banned on all public gathering, 53 member states have closed down all it school, 19 has placed limits on prisons and hospitals visitation, 15 currently engaging in mass screening and testing and has initiated and encourage public use of face mask/cloth. On restriction of movement, 32 countries have implemented night time curfews thus a restriction during a period of time in the affected area or nationally with 10 implementing curfews only and 22 included lock-down additionally to curfews. 19 countries have instituted a partial lock-down which comprising restriction non-essential movement within an area in the country or area and 18 have initiated national lock with restriction of non-essential movement in the country.
In African settings, as compared to other continents, recent evidence suggests high and large COVID-19 epidemics are expected and expecting the continent to be a potential epi centre as it shift from Europe and America, in consistent with evidence available in a preprint by the Centre for Mathematical modelling of infectious diseases, London School of Tropical Medicine, has asserted that , African countries have fewer means to suppress transmission and manage cases, as such, self-isolation of symptomatic persons and general physical distancing are unlikely to avert very large epidemics, unless distancing takes the form of tight lock-down measures. Notwithstanding, both interventions had been described as helpful to mitigate the epidemic.
Shielding (Physical isolation in a dedicated building) of high-risk individuals can reduce health service demand and, even more markedly, mortality if it features high uptake and low contact of shielded and unshielded people, with no increase in contact among shielded people. Can the culture dynamics in Africa allow long use of such measures?
The centre continue to note that, Strategies combining self-isolation, moderate physical distancing and shielding will probably achieve substantial reductions in mortality in African countries. Temporary lock-downs (which delayed epidemics by about 3 months), where socio-economically acceptable, can help gain crucial time for planning and expanding health service capacity and infrastructure . This approach was taken by most countries and in Africa lasting not more than 30days in most cases perhaps due to the peculiarity of it member states economies.
Therefore, on February 14, 2020 the Economic Community of West Africa (ECOWAS) convene it emergency preparedness and response meeting in Bamako, Mali. Among 7 strategies and roadmap pointed out were;
- Strengthen coordination, communication, and collaboration amongst Member States in preparedness for Covid-19 epidemic, including cross-border collaboration
- Enhance surveillance and management measures for Covid-19, particularly at entry points – air, land and sea
- Step up communication to ensure that the public receives accurate, appropriate and timely information regarding the epidemic.
- Urgently strengthen critical national capacities for diagnosing and managing cases
- Develop a strategic cost effective regional preparedness plan based on Member States’ priorities for governments, partners, and the private sector support.
- Promote multi-sectoral national efforts using one-health approach to maximise impact.
VII. Implement robust measures to assure availability of critical medical supplies, including laboratory materials, and personal protective equipment in the region.
Although in a weak health care infrastructure and systems— health officials in the region and across Africa have been implementing precautionary measures across several countries for at least a month on onset of the disease outbreak.
In responding to the SARS-CoV-2 epidemic, The Africa CDC has established the Africa Task Force for Novel Coronavirus (AFCOR). The Task Force is known to have made up of five working groups which are; disease surveillance, including screening at points of entry; infection prevention and control in healthcare facilities; clinical management of persons with severe 2019-nCoV infection; laboratory diagnosis and subtyping; and risk communication and community engagement. The group will also include representatives of Member States, WHO, and other subject matter experts and partners.
Other activities implemented by the continent CDC included a training on laboratory diagnosis of the 2019-nCoV for 15 African CDC Member States; initiating a specimen transport and referral system; training on surveillance, screening, isolation, and safe transportation of suspected cases for staff working at high volume airports in the continent; provision of testing supplies for selected laboratories in Africa that have the capacity to test.
Generally in Africa, (Ahmad and Komai, 2015) has presented that there are fewer Biosafety Level 3 and 4 (BSL-3, 4) laboratories in developing countries as compare to in developed countries. As such, it is imperative to establish more laboratories in Africa or increase the number of regional laboratories. The findings has it that, as at 2015, there are only two BSL-4 laboratories present in Africa and only three African countries have standard BSL-3 laboratories ( http://fas.org/ )However, The WHO Emerging and Dangerous Pathogens Laboratory Network (EDPLN) survey in 2016 indicated 11 BSL-3 Laboratory capacity to be present in Africa although having 14 members in the EDPLN. The following countries where reported to have had the BSL-3 hence participated in the survey, namely; Algeria, Uganda, Cameroon, Ghana, Nigeria, Gabon, Central African Republic, Madagascar, Senegal and South Africa.
In Ghana, as measures have been put in place, Government intended to achieve five (5) key objectives and that is;
- limit and stop the importation of the virus;
- contain its spread; provide adequate care for the sick;
- limit the impact of the virus on social and economic life;
- And inspire the expansion of our domestic capability and deepen our self-reliance.
Ghana as of May 13, 2020, 01:00 UTC, has recorded a total of 5,127 SARS-CoV-2 confirmed cases with 494 death and 22 deaths as reported by the Ghana Health service via https://www.ghanahealthservice.org/covid19/ but more new infection cases are being recorded on daily basis with a weekly infection growth rate at 75% as reported by United Nations Economic commission for Africa report.
A case fatality rate is the number of reported deaths per number of reported cases. Large differences in testing, reporting and categorization across countries, and data collection delays in such a highly dynamic situation as a result, estimated case fatality rates for COVID-19 vary widely across the world.
Data available proves that, Côte D’Ivoire, Djibouti, Ghana, Guinea and South Africa all have fatality rates below 2%. In North Africa, Algeria and Egypt have estimation case fatality rates of 11.5 per cent (%) and 7.2% respectively, swinging them among the apical 12 countries worldwide in terms of fatality rates. In the meantime, Cameroon, Morocco and Nigeria relatively exhibit case fatality rates as about 3%. What is needed is active learning: investing the resources and time needed to actively collect the data on this critical issue. In the light of this, More African countries need to collect and publish detailed testing and case data.
Ghana have succeeded in halting any more importations of the virus into the country by closing it borders and imposes international travel restrictions. The country as of now do not operate a national airline or carrier hence appears to be at a better side at enforcing such restrictions. Among other safety measures, the government has closed all schools and banned all social activities including religious and funeral rites as indicated by the Africa CDC and the ECOWAS strategy. Although other member states of ECOWAS have started opening up their borders. As at the time of publication of this work, Ghana have conducted over one hundred thousand test and has contact traced, isolate and quarantine infected individuals.
Although since independence, Ghana do not have a specialize infectious disease management and treatment centre in the wake of this SARS-CoV-2 pandemic, The testing have been spearheaded by the Noguchi Memorial Institute for Medical Research (NMIMR), a WHO Emerging and Dangerous Pathogens Laboratory Network (EDPLN) member reference lab, in the University of Ghana. To inspire the expansion of the domestic capability and deepen self-reliance as one of strategic measures, the country have been engage in mass production of Personal Protective Equipments (PPEs), among other; face shield and masks, alcohol base hand sanitizers, glovers, clinical scrubs, boots etc hitherto this where products largely imported. Employing non-pharmacology method being applied by several countries I.e social distancing rule, limiting funeral and burial functions to only 25 attendant, hand-washing hygiene protocols, exercises, drinking a lot of water and eating fruits and vegetables. The population seems to have defy social distancing rules as to some extent interview with some individuals shows that, they do not believe in the existence of the diseases rather claimed the government could have fabricated such ideas as the outbreak of diseases. This is evident to the fact that illiteracy rate among Ghanaians is still high and also could be largely attributed to the lack of education concerning Covid-19, failure on the side of the media to frequently educate the public in the right languages and lack or low level of trust in the system or public/government officials by the Ghanaian citizens.
To know the true extent of Ghana’s SARS-CoV-2 infection, it will be appropriate for the government to take a multi-facet approached not to lift the banned on social gatherings any time soon, schools continues to closed until taking the step to mass test at least 10% (estimations of 3 million individuals drawn from all the regions) of total population.
The Centre for Mathematical modelling of infectious diseases, London School of Tropical Medicine has modelled that assuming no mitigating strategy was developed Incident Cases between 93-120 days maybe at 270,000 – 490,000 and between 100-140days, Hospital Demand maybe 130, 000 – 220,000, Noncritical Demand maybe 89000 to 14000, Critical cases Demand 45000 -73000 and death cases could be recorded 2900 to 4500 at between 110 to 150 days. See the tables below. (Click here to download model)
Table 1: Overview of estimated peak impacts based on the population in Ghana. Rates of symptoms and severe outcomes are based on global outbreak data, which have primarily been observed in Asia, Europe, and North America. Timing is in days from initial introduction to Ghana.
| Outcome | Peak Day IQR (95% interval) | Peak Number IQR (95% interval) |
| Incidence of Symptomatic Cases | 93 120 (81 220) | 270K 490K (98K 560K) |
| All Hospital Demand | 100 140 (95 220) | 130K 220K (45K 270K) |
| General Hospital Demand | 100 140 (95 220) | 89K 140K (30K 180K) |
| Critical Care Demand | 100 140 (95 230) | 45K 73K (16K 92K) |
| Incidence of Deaths | 110 150 (100 240) | 2.9K 4.5K (1K 5.4K) |
Table 2: Peak timing and values for main outcomes in Ghana for the unmitigated scenario, by age group. Timing is days from the date of initial introduction.
| Peaks | Age Group | Peak Day, IQR (95% interval) | Peak Number, IQR (95% interval) |
|
Incident Cases |
all ages
<14 years 1529 years 3044 years 4559 years 60+ years |
93 120 (81 220)
95 130 (84 210) 96 120 (81 210) 89 120 (79 200) 94 120 (81 210) 96 130 (84 210) |
270K 490K (98K 560K)
80K 140K (25K 190K) 71K 120K (24K 160K) 71K 110K (24K 150K) 46K 80K (16K 100K) 18K 32K (5.5K 38K) |
|
Hospital Demand |
all ages
<14 years 1529 years 3044 years 4559 years 60+ years |
100 140 (95 220)
100 140 (96 220) 100 140 (93 220) 100 140 (91 220) 100 140 (93 220) 110 140 (97 220) |
130K 220K (45K 270K)
5.5K 8.3K (1.7K 12K) 5.6K 8.5K (2.1K 12K) 16K 26K (6.3K 33K) 44K 75K (16K 90K) 60K 110K (18K 130K) |
|
Noncritical Demand |
all ages
<14 years 1529 years 3044 years 4559 years 60+ years |
100 140 (95 220)
100 140 (96 220) 100 140 (93 220) 100 130 (91 220) 100 130 (92 220) 110 140 (96 220) |
89K 140K (30K 180K)
3.5K 5.5K (1.1K 7.4K) 3.9K 6.1K (1.3K 7.4K) 11K 17K (4.2K 22K) 28K 49K (10K 59K) 39K 69K (12K 80K) |
|
Critical Demand |
all ages
<14 years 1529 years 3044 years 4559 years 60+ years |
100 140 (95 230)
100 140 (100 230) 100 140 (93 220) 100 140 (92 220) 100 140 (93 220) 110 140 (97 220) |
45K 73K (16K 92K)
1.8K 2.9K (570 3.9K) 1.9K 2.9K (710 3.7K) 6.1K 8.9K (2.1K 12K) 15K 25K (5.7K 31K) 20K 36K (6.5K 42K) |
|
Incident Deaths |
all ages
<14 years 1529 years 3044 years 4559 years 60+ years |
110 150 (100 240)
110 150 (100 230) 110 140 (100 230) 110 150 (100 230) 110 150 (100 230) 110 150 (100 240) |
2.9K 4.5K (1K 5.4K)
110 180 (47 250) 110 180 (53 240) 380 520 (140 680) 970 1.5K (370 1.9K) 1.2K 2.2K (410 2.6K) |
Intervention Scenarios
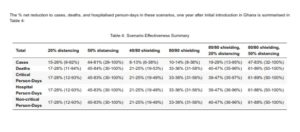
The panels in table 3 compare unmitigated epidemics with 5 different potential interventions in Ghana. The at 95% intervals (thus 95% certainty) for peak timing and values for those outcomes, the table below shows the relative trajectories in total outcomes, covers cumulative reductions due to the interventions at 3, 6, 9, and 12 months from initial introduction, estimation of introduction infection from onset being 50 initial infection. Note that these reduction may rise and decline with time as some interventions have large initial impact by delaying an epidemic, but ultimately many of the cases still happen.
The centre therefore hypothesize that;
- General physical distancing was implemented as a reduction in contacts, and thus transmission, for all interactions outside the household therefore, assumed no change in transmission within the household.
- Shielding was implemented by stratifying the population in one shielded and one unshielded compartment. Shielding applies to those aged 60+ years. They assume shielding of this population has a coverage fraction, and reduction fraction and hence refer to shielding interventions by coverage / reduction, so “80/80 shielding” is 80% coverage of 80% contact reduction. The centre show results for 40/80 and 80/80 here. In Ghana, 80% coverage corresponds to 1.3M individuals or 4% of the population, with half of those values for 40% coverage.
- To be effective, shielding must be maintained until the epidemic is over and must ensure that there is not substantially increased mixing amongst the shielded population.
Table 3 – See results below if interventions were to be instituted and maintain.
To enhance pandemic surveillance, mass testing and to meet the demand of the large samples being received, the NMIMR has employed the ‘pooling sample PCR analysis strategy’. The strategy is scientifically validated by WHO base on (Deckart et al, 2020) simulation study. Similar strategy is being used by the Standford’s Clinical Virology Laboratory and Tecnion – Israel Institute of Technology/Rambam Health Care as scientist say this serves as a valuable technique for future pandemic though not regarded as scientific breakthrough but a demonstration of using available equipments and method to significantly increase the volume of samples being tested per day indicating innovation confirmed by Professor Uri Sivan at Tenhnion.
CHALLENGES IN GHANA
In Ghana, Contact tracing although is on-going, the competency of the personnel involve in such activity has been question as this is evident in the laboratory at Noguchi. Some of the samples brought to NMIMR contain the following errors, lack of contact tracing forms/laboratory request forms attached to the individual samples collected, improper labelling of sample containers, improper or absence of required information on both the individual laboratory request form and misrepresentation of labelling on sample containers as some of the labels do not correspond to attached request form. This left such samples with the errors untested not discounting the possibilities of some of the samples to be positive leaving such individuals status unnoticed hence affecting and promoting horizontal transmission/community spread.
It’s therefore very imperative for the health ministry to adequately train such personnels and or transfer powers to NMIMR to handle and train the contact tracing team.
What we know about SARS-Cov-2
The novel coronavirus currently in circulation is a member of the family Coronaviridae. Until the discovery of the new novel coronavirus, six coronaviruses known to infect humans were the alpha coronaviruses 229E and NL63 and the beta coronaviruses OC43, HKU1, SARS-CoV, and MERS-CoV.
All known coronaviruses were isolated from animals and infect animals than humans with some infecting more than one different species of animals.
The new coronavirus SARS-Cov-2 like other members of the family is enveloped with unsegmented single-stranded positive sense RNA with a pleomorphic (appearing in different forms) and circular structure measuring about 60-140 nm in diameter.
According to the Chinese scientists the whole sequenced genome SARS-Cov-2 showed 96.2% similarity to SARS-related coronavirus and <80% similarity to SARS-CoV isolated from bats in China. Scientists from the University of Ghana are the latest to sequence the genome of SARS-Cov-2 circulating in Ghana as way to strengthen their surveillance effort. All 15 genomes as asserted by the University of Ghana in greater extents resembled (with > 92% similarity) the reference strain that was isolated in Wuhan, China. Signifying the genetic strain has not significantly change as the country is battling with the same pathogen the rest of the world is battling against. Scientist at Senegal’s Institute de Pasteur has developed simple cost effective test kit to test for the infection as it record lower death rate and being adjudged to have been the third in the world to have high recovery rates.
The virus is believed to have jumped species from animals to humans and now been transmitted between humans through respiratory droplets from coughing, sneezing, spitting and aerosol generating procedures by clinicians. On the other hand, scientist including public/Global health professionals believes the virus might have had an intermediary host before jumping onto human hence are researching this possible phenomenon. With an incubation period of 7 to 14 days, asymptomatic carriers are reported to be the major source of transmission. As of April 24, 2020, the epi centre of the disease remained the european region as it moves from China probably through stringent public health measures including testing. Meanwhile, A research letter reports on the prevalence of COVID-19 in 408 people among a homeless community in Boston. Findings report a 36% positivity rate and that 87.8% were asymptomatic. These results suggest that symptom screening may not adequately capture the extent of the disease transmission in high risk settings.
Immunity, treatment and vaccines
No group of people has demonstrated immunity against SARS-Cov-2 even though data available shows high fatalities among victims aged > 60years and people with serious underlining health condition with no fatality recorded among children under 10. The increased risks of death among the aged have been attributed to reduced immunity to infectious diseases due to aging and co-morbidities.
Nonetheless, whether people develop immunity to SARS-CoV-2 after being infected once remains has become a challenging question for Global/Public health experts, policy makers in various countries and everyone affected by the spread of the Covid-19 pandemic. A study in macaques monkeys provide a hint about such phenomenon. According to a Bao et al and published by www.the-scientist.com, Three rhesus monkeys did not develop a second infection after recovering from a first exposure of SARS-CoV-2 virus and re-exposed to the coronavirus, alluding that primates are capable of developing at least short-term immunity to the virus. On the other hand, the research is not clear how long the protection last and whether the antibody surge the researchers observed is part of the initial stage when antibody levels are still dropping off, rather than a true memory response. In-spite of this immune outcome, it still raise the question of why some COVID-19 survivors recovering and being discharged upon testing negative for the virus, only to then develop another infection. In perspective, this anomaly could be a result of suspected false-negative PCR testing or otherwise this remain one of the numerous questions that needs an answer.
Recent among them is Madagascar discovering possible treatment spearheaded by the Malagasy Institute of Applied Research. The Africa CDC has taken the steps to collaborate for more clinical trials to establish the drug efficacy while countries such as Senegal, Tanzania, Ghana, Kenya among others has supported the outcome. The WHO has also encourage more clinical trials into Madagascar’s Covid-Organic (the treatment developed) although continue to warn the world not to consume any untested remedies for Covid-19. The Noguchi Memorial Institute for Medical Research in Ghana is also noted to be researching into herbal/organic remedy as well.
A trial sponsored by the US National Institute of Allergy and Infectious Diseases (NIAID) with 1,063 hospitalized patients with advanced COVID-19 treated with remdesivir, reports that patients who received remdesivir had a 31% faster time to recovery than those who received placebo. The median recovery time was reduced from 15 days to 11 days in the patients receiving remdesivir, however there was no significant differences in survival. Following this, the U.S Food and Drug Administration issued an emergency use authorization for remdesivir for the treatment of suspected or laboratory-confirmed COVID-19 in adults and children hospitalized with severe disease.
A retrospective, observational cohort Dutch study of 95 COVID-19 patients has also suggests that treatment of COVID-19 patients with chloroquine resulted in a statistically significant and clinically relevant effect on the QTc interval. It is recommended that QTc intervals be monitored by recording a baseline electrocardiogram (ECG) and then a further ECG during chloroquine treatment. Meanwhile. a prospective, observational study of 201 hospitalized patients treated with chloroquine/hydroxychloroquine ± azithromycin, suggest no instances of Torsade de pointes (TdP) or arrhythmogenic death, although the maximum QTc during treatment was significantly longer in the combination group (chloroquine/hydroxychloroquine and azithromycin) vs. the monotherapy group (chloroquine/hydroxychloroquine). Although use of these medications resulted in QT prolongation, clinicians seldomly needed to discontinue therapy. Further study of the need for QT interval monitoring is needed before final recommendations can be made.
A study of 21 severe or critical COVID-19 patients treated Tocilizumab reports that within 5 days after tocilizumab, 75% of the patients had lowered their oxygen intake and CT scans manifested that the lung lesion opacity absorbed in 90.5% of the patients. The preliminary data suggests that tocilizumab, improved the clinical outcome immediately in severe and critical COVID-19 patients, suggesting it is an effective treatment to reduce mortality.
A retrospective cohort study of 46 severe patients with COVID-19 compared the clinical outcomes of COVID-19 pneumonia patients with or without methylprednisolone treatment. Findings suggest early, low-dose and short-term application of methylprednisolone was associated with better clinical outcomes in severe patients with COVID-19 pneumonia, and should be considered before the occurrence of ARDS. Nevertheless, future randomized controlled trials are desperately in need to confirm these findings and further study the mid- and long-term outcomes after discharge.
In a case study of 6 COVID-19 subjects with respiratory failure received convalescent plasma at a median of 21.5 days after first detection of viral shedding, all tested negative for SARS-CoV-2 RNA by 3 days after infusion, and 5 died. Findings suggest that convalescent plasma treatment can discontinue SARS-CoV-2 shedding but cannot reduce mortality in critically end-stage COVID-19 patients, and treatment should be initiated earlier.
The seemingly no recorded fatality among children under 10years remain a question yet to be unravelled by the scientific community, although two cases of babies being born with Coronavirus have been reported in March 2020. In both cases, it remains unclear whether the two babies infection was prior to, or soon after birth. Alternatively, Dr. David Evans, has claimed that an unborn baby is most unlikely to be exposed to during pregnancy, per available research evidence as there have been no confirm cases of babies being infected in the womb hence asserted that transmission of the virus in babies are very likely to occur post-birth. Nonetheless, some assumptions have been made including a possible lack of testing in the age group and poor inflammatory response, either way research is ongoing and the question remains unanswered.
Pregnancy makes the pregnant woman vulnerable to many infections and increases their risk for respiratory infections and pneumonia. Researchers in China found that pregnant women with Covid-19 in their third trimester are more at risk for severe respiratory symptoms requiring ICU care than the general population. Researchers have ruled-out the possibility of trans-plancental infection as babies born to infected mothers tested negative for SARS-Cov-2.
Despite the high death rate (2.5%) by Covid-19, lesser than that of Ebola fatality rate at 60%, MERS and the 2003 SARS outbreak, it appears that efforts to find a definite cure for the deadly virus remains a challenge after several trials involving drugs already in use for the treatment of some medical conditions notably ACE -2 inhibitors, antivirals, antibiotics, antiparasitics and steroids. At present hydroxychloroquine appears to be most promising, as published by the international journal of antimicrobial activity, and as such is been used in many countries across the globe. However, the drug has been reported to have been causing Cardiovascular diseases conditions as well as brain damage hence needs review.
As of now, several vaccine candidates are in various phase of clinical trials among them is the U.S government collaborative effort with Johnson & Johnson in developing Ad26 SARS-CoV-2 9an investigational vaccine) and the Moderna SARS-CoV-2 MRNA-1273 which has passed through it phase 2 trials and currently undergoing phase 3 clinical vaccine trials. On this note, the Gilead pharmaceutical remdevir (antiviral has proven ineffective on SARS-CoV-2)
In Ghana, treatment protocols includes administering of vitamin C and proper feeding by the infected. The country has not yet categorically published or reveal it absolute treatment protocols.
With increasing spread of SARS-CoV-2 infection across the globe, there has been an increased interest in developing an effective SARS-CoV-2 vaccine that can protect the population. With the publication of the sequenced SARS-CoV-2 genome, research groups have been able to start SARS-CoV-2 vaccine adopting lessons from SARS and MERS vaccines development.
A phase 1 clinical trial of SARS-CoV-2 vaccine called mRNA-1273 funded by the National Institute of Allergy and Infectious Diseases (NIAID) ongoing at Kaiser Permanente Washington Health Research Institute (KPWHRI) in Seattle. Starting the first SARS-Cov-2 clinical trial, Dr. Lisa A. Jackson, senior investigator at KPWHRI remarked “This work is critical to national efforts to respond to the threat of this emerging virus” There is currently no vaccine against SARS-Cov-2. Some vaccines have reached Phase 3 clinical trials with some given orphan status
The Socio–economic implication of the Covid-19 pandemic
With the virus rapidly spreading and crossing borders, the most important strategy has been isolation and social distancing. As a result of which schools and business were closed. For many countries, movements were restricted and borders closed. The global economy has been heavily impacted through many interwoven factors including disruptions in global supply chains, supply shortages, increased prices of essential products, collapse of stock markets, massive laying-off of workers, unanticipated increase in health expenditure and decline in tourism including non-operations of airlines.
There has been massive economic distress even on the most advanced countries. For example a record of more than 3 million Americans are filing unemployment benefit claims and $2 trillion fiscal expansion package has been approved by congress to cushion the economy.
The economic impact of Covid-19 will yet hard hit African countries with already low industrial capacities. The United Nations Economic Commission for Africa (UNECA) has predicted a drop in Africa 2020 projected GDP growth from 3.2% to 1.8 % due to Covid-19. The World Bank also estimated a 1% decline in developing country growth rates will push as many as 20million people into poverty. The UNECA in their report ‘’COVID-19: Lockdown exit strategies for Africa’’ on May 2020, has further estimates that a one-month full lockdown across Africa would cost the continent about 2.5 per cent of its annual GDP, equivalent to about $65.7 billion per month. This is separate from and in addition to the wider external impact of COVID-19 on Africa of lower commodity prices and investment flows.
With much pressure on existing health infrastructure and health workforce, many Africans will suffer the diversion of attention from chronic and endemic infectious diseases such as malaria, HIV, Hypertension, Diabetes, Tuberculosis etc.
In Ghana, 214 cases and 33 deaths have occurred due to Cerebro-Spinal Meningitis (CSM) in the upper West Region of Ghana with a seemingly lack of attention. Dr. Rashid Pelpuo, Member of Parliament of Wa Central had to draw the attention of the Ministry of Health over the seemingly lack of attention of the menace.
Presenting his plea on the floor of Parliament he said “Currently there is an infectious disease in the Wa Central Constituency as well as in the Upper West Region as a whole. I wish to call on the Ministry of Health and the government to act with dispatch in providing immediately and adequately the essential grants needed, equipment and appropriate personnel to tackle this thriving danger. This is a crucial time and especially because CSM is a very infectious disease but may be grossed over by the authorities and the people themselves given the present situation we find ourselves,”
It is clear that Covid-19 pandemic has shaken the entire world affecting both lives and the economy but as the President of the Republic of Ghana said “We can bring economy back to life but we can’t bring the dead back to life”, we can only hope to recover stronger to rebuild our economy and health care infrastructure.
Additionally, to help set research agenda, some legitimate questions remain Unanswered, as follows:
- Could SARS-Covid-2 be a bioweapon or incidental escaped from a laboratory?
- How does children under 10years relatively less affected?
- Is there any possibility for Adaptive immunity after?
- How will lessons learnt from Covid-19 affect the global community?
- Is there any cross immunity advantage to Africans?
- Why are Africans still relatively less affected?
- Could the total cases in Africa possibly be a true reflection of the actual infection rate across the Africa CDC member states or an issue of under reporting of cases perhaps due to logistical reasons and non-availability of resources, intentional or unintentional with-holding of confirmed cases figures by governments and or due to tropical climate condition in sub-sahara Africa?
Authors:
Edem, Nukunu (BS, MD)1 & Kwame Sherrif, Awiagah (BSc, MPhil)2
- He was an intern at Noguchi Memorial Institute for Medical Research (NMIMR) and currently serves as volunteer Scientist for SARS-CoV-2 at NMIMR . He is also a member of the Medical Journalists’ Association – Ghana and a member of the World Federation of Science Journalists as well as a member of the Global Emerging-Pathogen Treatment (GET) Consortium. (PLUS Faculty). Reach out for him via correspondent e-mail: [email protected]
- He is Medical Virologist, Senior Nurse at Korle-Bu Teaching Hospital and a member of the Medical Journalists’ Association – Ghana. Reach out for Him via [email protected]
References
- https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html
- https://www.who.int/health-topics/coronavirus
- Anjorin A. The coronavirus disease 2019 (COVID-19) pandemic: A review and an update on cases in Africa. Asian Pac J Trop Med 2020; 13: 10.4103/1995-7645.281612
- Bao et al., ‘’Reinfection could not occur in SARS-CoV-2 infected rhesus macaques’’.bioRxiv. Doi:10.1101/202.03.13.990226, 2020
- https://www.dailmail.co.uk/health/article-8137899/Are-looking-wrong-symptoms-bid-beat.html
- https://www.worldometers.info/coronavirus/
- Asian Pac J Allergy Immunol 2020;38:1-9 DOI 10.12932/AP-200220-0772
- Hussin A. Rothan and Siddappa N. Byrareddy, Journal of Autoimmunity, https://doi.org/10.1016/j.jaut.2020.102433
- wahooas.org
- https://m.dw.com/en/coronavirus-how-africa-has-been-preparing-for-outbreak/a-52576674
- https://ln2.sync.com/dl/b3fc9ebc0?sync_id=1394099265#36ipcgk3-5mghvhh4-vi29b9yy-8e688twu
- https://ln2.sync.com/dl/b3fc9ebc0#36ipcgk3-5mghvhh4-vi29b9yy-8e688twu
- https://cmmid.github.io/topics/covid19/LMIC-projection-reports.html
- https://cmmid.github.io/topics/covid19/covid-response-strategies-africa.html
- https://africacdc.org/news-item/africa-cdc-establishes-continent-wide-task-force-to-respond-to-global-coronavirus-epidemic/#
- Decert A, Barnighausen T & Kyei N. Pooled-sample analysis strategies for COVID-19 mass testing; a simulation study (preprint). Bull World Health Organ. E-pub: 2 April 2020. doi: http://dx.org/10.2471/BLT.20.257188
- standford.edu/news/all-news/2020/04/testing-pooled-samples-to-track-early-spread-of-virus.html
- com/news/2020-03-pooling-method-dozens-covid-simultaneously.html
- https://www.aljazeera.com/news/2020/05/coronavirus-madagascar-herbal-remedy-covid-19-organics-20050513105598.html
- WHO Africa (2016). Report on the Status of EDPLN BSL-3 in Select Countries in the African Region.
- Ahmad A & Komai Are developing countries prepared to face Ebola-like outbreaks? Article in Virologica Sinica June 2015 DOI: 10.1007/s12250-015-3564-9
- Africa CDC and Member States – Preliminary Summary of Information. COVID-19 Scientific and Public Health Policy Update – (05 May 2020)
- Harvard University Center for International Development, “Smart containment with active learning: a proposal for a data-responsive and graded response to COVID-19” (Cambridge, Massachusetts, 2020). Available at hks.harvard.edu/centers/cid/publications/smart-containment-with-active-learning
- Centre for Evidence-Based Medicine, “Global COVID-19 case fatality rates” (Oxford, CEBM Research, Oxford COVID-19 Evidence Service, 2020). Available at cebm.net/covid-19/global-covid-19-case-fatality-rates/.
- https://www.un.org/africarenewal/news/coronavirus/eca-proposes-covid-19-exit-strategies-bring-african-economies-back-track
- United Nations Economic Commission for Africa. ‘’Covid-19 lockdown exit strategies for Africa’’, May 2020. Available at https://www.uneca.org/publications/covid-19-lockdown-exit-strategies-africa
Columnist: P. Edem, Nukunu1 & K. Sherrif, Awiagah2




Comments are closed.